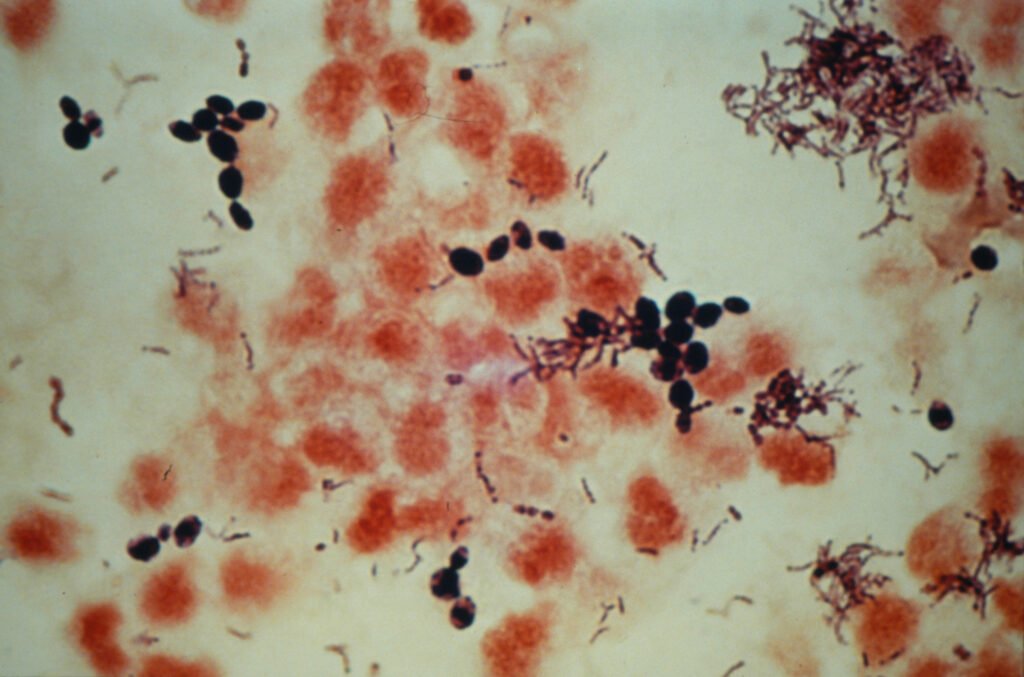
Candida glabrata is a species of yeast that belongs to the genus Candida, a group of fungi that are normal inhabitants of human mucosal surfaces, including the gastrointestinal tract, vagina, and skin. While the human microbiome typically maintains a balanced environment, certain conditions can lead to an overgrowth of Candida species, including Candida glabrata, transforming them from benign commensals into opportunistic pathogens.
One of the distinguishing characteristics of Candida glabrata is its genetic makeup, which predisposes it to various forms of resistance against antifungal medications, distinguishing it from more common strains such as Candida albicans. Unlike Candida albicans, which is often associated with localized infections such as thrush or vaginal yeast infections, Candida glabrata is particularly notable for its ability to cause systemic infections, especially in immunocompromised individuals. This unique pathogenic potential raises concerns in clinical settings, as its increasing prevalence poses significant challenges in treatment.
In healthy individuals, Candida glabrata typically exists without causing any harm; however, in certain circumstances such as prolonged use of antibiotics, surgical interventions, or immunosuppressive therapy, this yeast can proliferate uncontrollably, leading to infections. The susceptibility of immunocompromised patients to Candida glabrata infections accentuates the importance of monitoring and managing this organism in healthcare environments. Within this context, healthcare providers must remain vigilant regarding both its potential implications for patient health and the evolving antifungal resistance landscape.
In sum, understanding Candida glabrata and its role in human health is crucial for developing effective treatment strategies for infections attributed to this opportunistic pathogen. Its differentiation from other Candida species highlights the complexity of fungal infections and the need for ongoing research and surveillance.
Symptoms and Risk Factors of Candida Glabrata Infections
Infections caused by Candida glabrata can manifest in various forms, depending on the location within the body. Commonly, these infections may occur in the bloodstream, urinary tract, or mucosal surfaces. Symptoms of bloodstream infections often include fever, chills, and a general feeling of malaise. Patients may present with sepsis, a severe condition that arises when the body’s response to infection damages its tissues and organs. Urinary tract infections may lead to discomfort while urinating, frequent urges to urinate, and lower abdominal pain. If the infection affects mucosal areas, symptoms may include itching, burning sensations, or unusual discharge, particularly in cases such as vulvovaginal infections.
Understanding the risk factors that increase the likelihood of developing Candida glabrata infections is crucial for prevention and early treatment. Individuals with underlying health conditions, such as diabetes, are particularly vulnerable due to compromised immune responses and potential disruptions in blood glucose levels that favor fungal growth. The use of broad-spectrum antibiotics can also alter the natural flora of the body, reducing competition for Candida species and allowing Candida glabrata to proliferate. Furthermore, patients undergoing immunosuppressive treatments, including those for cancer, organ transplants, or autoimmune diseases, are at heightened risk. These treatments weaken the immune system’s ability to combat infections, making it easier for Candida species to establish infections.
Other risk factors include age, with elderly individuals facing a higher inclination to infections due to weakened immunity, and prolonged hospital stays, where the risk of exposure to resistant strains increases. By recognizing these symptoms and risk factors associated with Candida glabrata, individuals and healthcare providers can take necessary precautions and respond promptly to prevent severe complications.
Diagnosis and Treatment Options for Candida Glabrata
The diagnosis of Candida glabrata infections typically involves a combination of clinical evaluation and laboratory testing. Healthcare providers begin by assessing the patient’s symptoms, which may vary based on the site of infection. Common presentations include vaginitis, urinary tract infections, and systemic infections, particularly in immunocompromised individuals. Accurate diagnosis is crucial, as Candida glabrata is known for its resistance to numerous antifungal agents that are effective against other Candida species.
Laboratory tests play a vital role in confirming the presence of this yeast. One of the most commonly used methods is culture testing, where samples from the affected area, such as blood, urine, or vaginal secretions, are cultured on appropriate media to identify Candida glabrata. Molecular techniques, such as polymerase chain reaction (PCR), are also increasingly utilized, providing rapid and sensitive identification of the organism. These advanced methods are particularly beneficial for diagnosing resistant strains, ensuring appropriate treatment strategies are implemented promptly.
Treatment options for Candida glabrata infections are multifaceted and often require a tailored approach. Standard antifungal therapies include azoles, echinocandins, and polyenes. However, it is important to note that Candida glabrata exhibits inherent resistance to azole medications such as fluconazole. Consequently, healthcare providers must carefully select antifungal agents, considering the individual patient’s health status, potential drug interactions, and resistance patterns. For patients with recurrent infections, it may be necessary to employ combination therapy or explore newer antifungal options.
Beyond treatment, strategies for managing and preventing reinfections are essential. Patients are advised to maintain good hygiene, manage underlying health conditions, and consult their healthcare provider for regular assessments. In conclusion, understanding the diagnostic landscape and treatment options for Candida glabrata is pivotal for effective management and improved patient outcomes.
Prevention and Lifestyle Tips to Manage Candida Glabrata
Managing the risk of Candida glabrata infections involves a combination of lifestyle changes, dietary adjustments, and measures aimed at strengthening the immune system. By adopting these strategies, individuals can create an environment less conducive to yeast overgrowth.
A significant part of prevention lies in dietary choices. It is advisable to limit the intake of sugar and refined carbohydrates, as these can contribute to the proliferation of Candida species, including Candida glabrata. Instead, focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Foods such as garlic, olive oil, and fermented products, such as yogurt or kefir, can support a healthy gut flora, inhibiting yeast growth. Including prebiotic and probiotic foods can also enhance your digestive health. Probiotics, in particular, can help restore the natural balance of bacteria and fungi in the body, which is essential in managing conditions associated with Candida.
Additionally, maintaining a healthy immune system is crucial in preventing infections. Adequate sleep, regular physical activity, and stress management techniques—such as mindfulness or meditation—can bolster immune function. Avoiding excessive use of antibiotics is also essential as these can disrupt the natural microbiome, paving the way for opportunistic infections like those caused by Candida glabrata.
Regular health check-ups play an important role in monitoring overall health and detecting any potential issues early on. If you notice any unusual symptoms, such as recurring yeast infections or unusual digestive issues, consult a healthcare professional promptly. Early intervention can make a significant difference in managing Candida glabrata effectively.